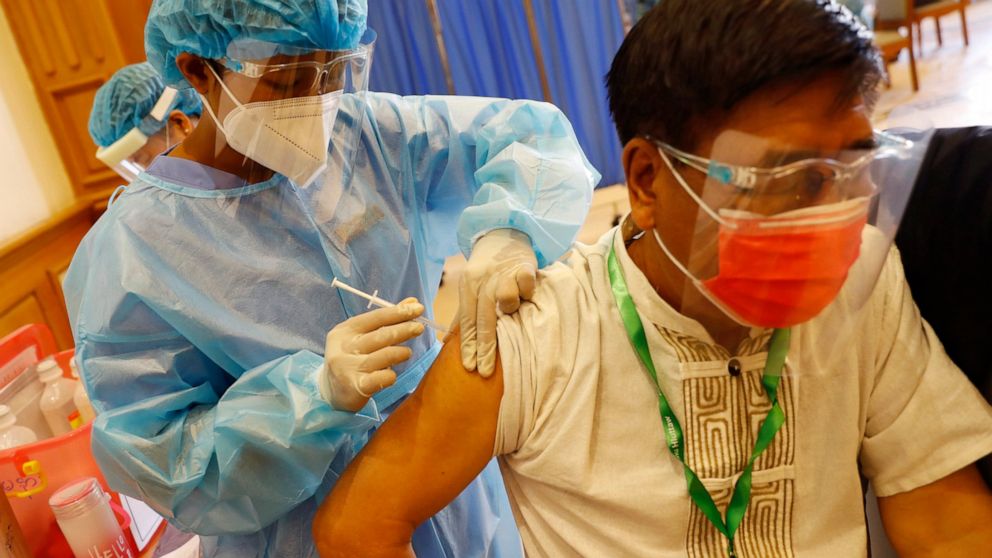
Photo courtesy of ABC News
Sri Lanka, although facing challenges related to vaccination coordination, has started vaccinating the public. As misinformation can be a serious challenge to understanding the vaccine landscape during this crucial time, here is a brief guide on vaccines, their global availability and why public health measures are still important.
As of February 27, 2021, globally there are 74 vaccines in clinical development and 182 vaccines in pre-clinical development. There are so many vaccines developed within a short period of time and so many conflicting news stories it can be difficult to keep up.
What are the major vaccines in use?
Currently, there are four main approved vaccines from four different developers. These vaccines include vaccines developed by Pfizer and BioNTech (Comirnaty), Moderna (mRNA-1273), Astra-Zeneca, and Oxford University (Covishield) and Gamaleya Research Institute of Russia (Sputnik V). Vaccines by Pfizer and BioNTech and the vaccine by Astra Zeneca and Oxford University are also approved by the World Health Organization’s (WHO) Strategic Advisory Group of Experts on Immunization (SAGE). The following table provides the basics of these four vaccines.
| Developer | Vaccine name | Efficacy | Optimal period between shots | Storage temperature | Approved countries |
| Pfizer and BioNTech | Comirnaty | 95% | 3 weeks | Freezer storage (–25°C to –15°C) | Approved: Bahrain, Brazil, New Zealand, Saudi Arabia, Switzerland
Approved for emergency use: Argentina, Australia, Canada, Chile, Colombia, Costa Rica, Ecuador, European Union, Hong Kong, Iceland, Iraq, Israel, Japan, Jordan, Kuwait, Lebanon, Malaysia, Mexico, Mongolia, Norway, Oman, Panama, Peru, Philippines, Qatar, Serbia, Singapore, Tunisia, United Arab Emirates, United Kingdom, United States Approved by WHO’s SAGE Working Group for emergency use |
| Moderna | mRNA-1273 | 94.5% | 4 weeks | 30 days with refrigeration; six months at -20°C freezer temperature | Approved: Switzerland.
Approved for emergency use:Canada, European Union, Iceland, Israel, Mongolia, Norway, Qatar, Singapore, United Kingdom, United States. |
| Astra-Zeneca and Oxford University | Covishield | 82.4% | 12 weeks | Stable in refrigeration temperature for at least 6 months | Approved for emergency use:Algeria, Argentina, Australia, Bangladesh, Bhutan, Brazil, Chile, Dominican Republic, Egypt, El Salvador, European Union, Iceland, India, Iraq, Kuwait, Maldives, Mexico, Mongolia, Morocco, Nepal, Nigeria, Norway, Pakistan, Philippines, Saudi Arabia, Seychelles, Sri Lanka, South Africa, South Korea, Thailand, United Kingdom, Vietnam
Approved by WHO’s SAGE Working Group for emergency use |
| Gamaleya Research Institute of Russia | Sputnik V | 91.6% | 3 weeks | Freezer temperature storage | Approved for early use: Russia
Approved for emergency use:Algeria, Argentina, Armenia, Bahrain, Belarus, Bolivia, Bosnian Serb Republic, Egypt, Honduras, Gabon, Ghana, Guatemala, Guinea, Guyana, Hungary, Iran, Kazakhstan, Kyrgyzstan, Lebanon, Mexico, Mongolia, Montenegro, Myanmar, Nicaragua, Pakistan, Palestinian Authority, Paraguay, San Marino, St. Vincent and the Grenadines, Serbia, Tunisia, Turkmenistan, United Arab Emirates, Uzbekistan, Venezuela. |
Source: World Health Organization, New York Times
In addition to the above four vaccines Johnson and Johnson has developed a single dose vaccine that has been approved for emergency use in Bahrain and in the United States. However, there are many other vaccines in the pipeline and approved in some countries such as vaccines by CanSino Biologics, Beijing Institute of Biological Products which do not have their research data of the phase 3 trials (clinical trials of vaccines that usually include thousands of human subjects) published.
How do these vaccines work?
Many of these vaccines have different mechanisms through which they build immunity in the body. The types of vaccines based on mechanism include:
- RNA/DNA based vaccines which build immunity via genetically engineered DNA/RNA fragments that help produce proteins that causes an immune response.
- Protein based vaccines that use harmless shells of proteins or parts of proteins that is similar to COVID-19 virus to build an immune response.
- Inactivated or weakened virus vaccines that does not cause the disease but creates an immune response to help protect against future infections.
- Viral vector vaccines which usually use a non-disease causing virus as a platform to deliver genes that create coronavirus proteins that help build an immune response.
Out of the listed vaccines above both Pfizer/BioNTech and Moderna vaccines are RNA based vaccines (using messenger RNAs also known as mRNAs), both AstraZeneca/Oxford and Gamaleya Research Institute vaccines are viral vector vaccines that use Adenovirus as the platform to deliver DNA strands to help build an immune response. If you are not a scientist but interested in the underlying science of the vaccines this 5 minute video by the WHO will give you further insight.
Although we have overcome the challenge of finding a vaccine that will help us against COVID-19, many challenges remain in terms of distribution and availability.
Why are vaccines not readily available?
Challenges such as not having enough vaccines due to production speed, inability to deliver vaccines due to storage facility and capacity shortcomings has created vaccine inequity. For example, of the four listed vaccines above, only Covishield by AstraZeneca/Oxford is stable for a long period in refrigerators. Many low and middle income countries do not have facilities to store and transport vaccines in freezer level temperatures – creating further challenges for these countries to deliver the vaccine to their populations.
Another major challenge, perhaps the most daunting, is vaccine hoarding by wealthier countries. Wealthier countries have made bi-lateral deals with vaccine production companies for large quantities of vaccines which significantly affect equal distribution of vaccines across the world. Currently, high income countries which accounts for 16 percent of the world’s population has purchased more than half of COVID-19 vaccines. Experts argue that for us to reach herd immunity (the target of vaccinating at least 70 percent of the population) rich countries need to donate vaccines even at lower levels. Otherwise, it could lead to a domino effect of inequality and inequity. For example, high income countries can impose travel restrictions citing low vaccination rates as a reason and delay in vaccination can also negatively impact the economies of less wealthy nations.
Are there mechanisms to provide vaccines to all?
The COVID-19 Vaccine Global Access (COVAX) is a mechanism co-led by the WHO, Gavi, the Vaccine Alliance, and the Coalition for Epidemic Preparedness Innovations. COVAX is one of the pillars of the ACT-Accelerator launched by the WHO to work collaboratively to accelerate COVID-19 diagnostics, treatments and vaccines. COVAX focusing on vaccines has set an initial goal to provide around 2 billion doses of vaccines to around 190 countries. Although, high income countries are part of COVAX, their direct deals with vaccine producing companies have created a short supply of vaccines for others. COVAX facility is however, moving forward with what they have and with increased support such as the US $4 billion recently pledged by the US. Ghana last week became the first country to receive vaccines under the COVAX facility. Globally, we have a long way to go.
What can we do?
As a middle income country with less buying power than a high income country, Sri Lanka will face delays in receiving vaccines for all. Therefore, first, as the public, it is crucial that we prioritize vulnerable groups such as those above 65 and frontline workers such as healthcare and social care workers. In other words, even if the distribution system is not functioning at its optimal level, you have a responsibility to give priority to those who are vulnerable. The second crucial step is that even after vaccination to continue using public health measures such as mask use, hand washing, hand sanitizing and maintaining recommended physical distancing. This is because vaccination does not give you complete protection against COVID-19 and there are chances of asymptomatic spread. Until we reach herd immunity, think of your protection and the protection of others, and continue to use public health measures.
From a government policy perspective, there is a clear challenge to address: the country is facing confusion with regard to priority groups, the coordination of vaccine administration and sadly the privileged are getting access to vaccines before the vulnerable. There is a massive need for coherent and updated policies with regard to local vaccine distribution that set out criteria for priority groups and vaccine distribution mechanisms. Sri Lanka is known to have a high functioning immunization system. Therefore, strengthening the system with clear guidelines, prioritizing vulnerable populations and shutting down backdoor access to the privileged will make a huge difference in our battle against COVID-19.
This is our crucial next step as a nation against the pandemic. As the public, let’s keeps our masks on, hands washed and allow the vulnerable to get vaccinated first; as the government address the need of the hour and provide clear policy guidance for vaccine administration. Every effort will count towards saving lives.
The author is formerly a Policy Associate at the Center for Policy Impact at the Duke Global Health Institute and is currently a Ph.D. candidate focusing on global health policy at McGill University. He tweets at @ShashikaLB